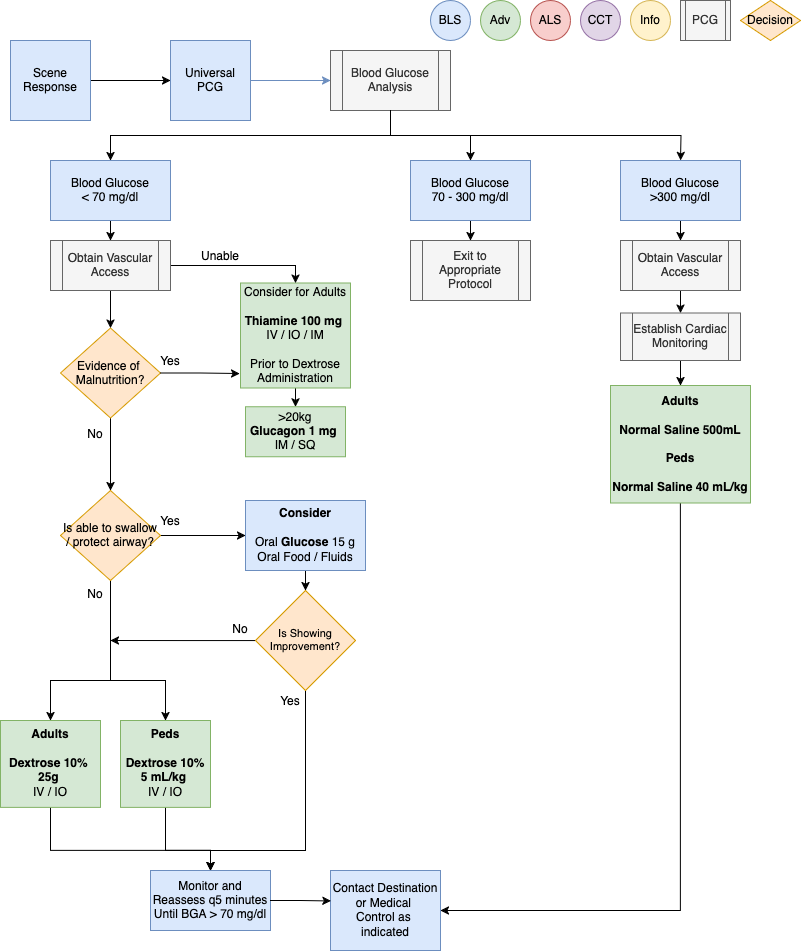
Diabetic Disorders
Applies to: Blood glucose less than 70 mg/dL or greater than 300 mg/dL **and**
- Patient-reported low or high blood glucose
- Diabetic patients with other medical symptoms (e.g., vomiting)
- Altered mental status
- Alcohol intoxication, suspected
- Seizure
- Stroke symptoms
- Unresponsive patients
- Cardiac arrest
Exclusion Criteria: None
History
- Past medical history
- Medications
- Drug allergies
- Last Meal
- Last BGA check
Signs and Symptoms
- Altered mental status
- Combative / irritable
- Diaphoresis
- Seizures
- Abdominal pain
- Nausea / vomiting
- Weakness
- Dehydration
- Deep / rapid breathing
Differentials
- Alcohol / drug use
- Toxic ingestion
- Trauma; head injury
- Seizure
- CVA
- Altered baseline mental status
Pearls
- Patient’s refusing transport to medical facility after treatment of hypoglycemia:
- Blood sugar must be ≥ 80, patient has ability to eat and availability of food with responders on scene.
- Patient must have known history of diabetes and not taking any oral diabetic agents.
- Patient returns to normal mental status and has a normal neurological exam with no new neurological deficits.
- Must demonstrate capacity to make informed health care decisions. See Universal Patient Care Protocol UP-1.
Otherwise contact medical control.
- Hypoglycemia with Oral Agents:
- Patient’s taking oral diabetic medications should be encouraged to allow transportation to a medical facility.
They are at risk of recurrent hypoglycemia that can be delayed for hours and require close monitoring even after
normal blood glucose is established. - Not all oral agents have prolonged action so Contact Medical Control or NC Poison Control Center for advice.
Patient’s who meet criteria to refuse care should be instructed to contact their physician immediately and
consume a meal.
- Patient’s taking oral diabetic medications should be encouraged to allow transportation to a medical facility.
- Hypoglycemia with Insulin Agents
- Many forms of insulin now exist. Longer acting insulin places the patient at risk of recurrent hypoglycemia even
after a normal blood glucose is established. - Not all insulins have prolonged action so Contact Medical Control for advice.
- Patient’s who meet criteria to refuse care should be instructed to contact their physician immediately and
consume a meal.
- Many forms of insulin now exist. Longer acting insulin places the patient at risk of recurrent hypoglycemia even
- Congestive Heart Failure patients who have Blood Glucose > 250:
- Limit fluid boluses unless patient has signs of volume depletion such as, dehydration, poor perfusion,
hypotension, and/ or shock.
- Limit fluid boluses unless patient has signs of volume depletion such as, dehydration, poor perfusion,
- In extreme circumstances with no IV / IO access and no response to glucagon, D50 can be administered rectally,
Contact Medical Control for advice.
Navigate
References
Protocols
Pharmacology
- Dextrose 10%
- Dextrose 50%
- Glucagon
- Glucose
Procedures
- Vascular Access
No Comments